Immigration Enforcement and Health Care Access
By Annie Hines, University of California, Davis
The recent pandemic has highlighted both health disparities across the U.S. and the importance of health care access. Health and health care access vary widely by racial and ethnic groups, geography, and socioeconomic status (E.g., Anderson et al., 2004s), as well as immigration status. While immigrants are typically healthier than the native population, they also face substantial barriers to health care access. This report discusses the impact of immigration enforcement on health care access for immigrants and their families.
Barriers to Health Care Access for Immigrants
Immigrants, particularly undocumented ones, face substantial barriers to accessing health care. They are also less likely to have insurance, relative to citizens, less likely to have a stable health care provider, and more likely to rely on the hospital or emergency room as their primary source of care (Martinez-Donate et al., 2014; Akresh, 2009; Vargas Bustamante et al., 2012). Transportation poses another barrier: undocumented immigrants are generally ineligible to obtain driver’s licenses, so simply getting to and from a doctor or hospital can be a challenge. The fear of being pulled over by the police while driving can also be a deterrent to seeking health care (Rhodes et al., 2015).
Immigration enforcement also affects immigrant health. Research shows that deporting undocumented immigrants from the U.S. affects the health and health care access of immigrants and their families remaining in the country (E.g., Wang and Kaushal, 2014; Watson, 2014). Fear generated by frequent deportations can cause stress for potential deportees, friends and relatives. This fear may lead immigrants, and even citizen family members, to alter their behavior to limit interactions with government authorities. This may include avoiding workplaces or community events, not signing up for public programs, or deferring health care to avoid the records and bureaucracy that, they fear, could lead to deportation. Currently, COVID-19 is revealing the public health consequences of immigrants avoiding medical facilities and health care out of fear of deportations or losing green card eligibility (Jordan, 2020).
Immigration Enforcement in the U.S.
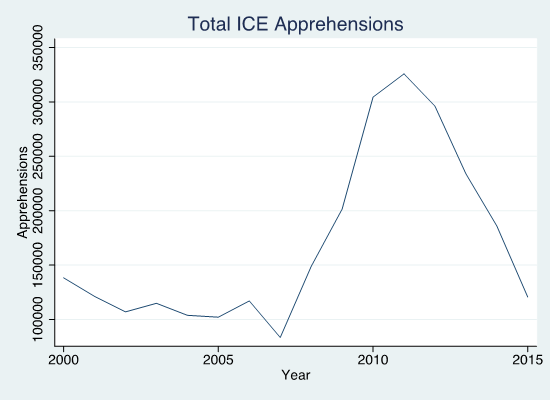
Over the past two decades, the U.S. has implemented important changes to its immigration policy. Who is allowed to cross the border? How do they access public programs, health care, and education once in the U.S.? Are those without authorization to live in the country forced to leave? These questions are part of a constantly evolving system of policies and laws implemented and enforced by and federal institutions. As part of a shift in federal policy towards a more aggressive stand on immigration enforcement, the Department of Homeland Security implemented the program Secure Communities (SC) in 2008. This program increased cooperation between local law enforcement and federal immigration authorities and led to a large increase in immigrant deportations (as shown in Figure 1). The program required local law enforcement to screen anyone booked into jail, no matter the reason, for immigration violations. Immigration and Customs Enforcement (ICE), the federal immigration enforcement agency, could then take custody of any person found to have violated immigration law. Between its introduction in 2008 and its temporary suspension in 2014, SC resulted in over 450,000 deportations (Hines and Peri, 2019). In addition to SC, some counties entered into 287(g) agreements during this period. These voluntary agreements deputized local police to enforce federal immigration law, including detaining people for suspected immigration violations. These programs increased the risk of deportation for undocumented immigrants by making interactions with local law enforcement, rather than immigration authorities, a potential cause for removal from the U.S.
Effects of Deportations on Health and Health Care Access
Prior studies document wide-ranging effects of immigration enforcement programs, from reducing immigrant educational attainment to increasing material hardship (Amuedo-Dorantes and Lopez, 2017; Gelatt et al., 2017). The effects of enforcement also extend to health care access and health outcomes, which respond to heightened enforcement through multiple channels. Research shows that deportations affect health outcomes directly by increasing stress (Venkataramani et al., 2017; Novak, Geronimus and Martinez-Cardoso, 2017; Wang and Kaushal, 2018; Lopez et al., 2017; Torche and Sirois, 2019; Cavazos-Rehg, Zayas and Spitznagel, 2007). Wang and Kaushal (2018) use the National Health Interview Survey (NHIS) to examine the effect of SC and 287(g) agreements, on the self-reported physical and mental health of Latino immigrants in the US (Wang and Kaushal, 2018). Analyzing the 2000-2012 period, they find that the implementation of SC led to a 14.7 percent increase in mental health distress for this group.
Deportations also have indirect effects on immigrant health and health care access. Recent work shows evidence that immigration affects the employment of low-educated non-citizens (East et al., 2018), which may also affect employer-sponsored health insurance. Heightened immigration enforcement affects participation in public programs, including the take up of public health insurance (Watson, 2014; Swartz et al., 2017; Rhodes et al., 2015; Vargas, 2015; Alsan and Yang, 2018). In health care, a variety of qualitative and interdisciplinary studies document how immigration enforcement may deter people from seeking health services, delay necessary care, or reduce the use of preventive care (Rhodes et al., 2015; Hacker et al., 2012; Lopez et al., 2017; Maldonado et al., 2013; Cavazos-Rehg, Zayas and Spitznagel, 2007). This research suggests that undocumented immigrants face substantial barriers to receiving health care, and immigration enforcement may increase these barriers.
Evidence of chilling effects in health care, where enforcement may deter those eligible for public programs from signing up, as well as qualitative work on spillover effects across communities makes it clear that citizens related to undocumented immigrants, or living in the same communities, also suffer the impacts of enforcement policies targeting undocumented immigrants (Asad and Clair, 2018). In one recent study, Alsan and Yang (2018) consider the effect of fear of deportations on take-up of the federal Supplemental Nutrition Assistance Program (SNAP) and health insurance enrollment under the Affordable Care Act (ACA). They focus on spillover effects on US citizens and find that the implementation of SC led to a decline in SNAP participation and ACA enrollment that are concentrated among mixed-status households. They also show a larger response in areas that are likely to have a higher fear of deportation and a smaller effect in sanctuary cities. Their main results suggest a ten percent decrease in Food Stamp take-up by Hispanic heads of households after the introduction of SC, relative to non-Hispanics. There was also a two percent decrease in Hispanic ACA sign-ups for every ten percent increase in detentions under SC.
Immigration Enforcement and Hospital Utilization
Despite substantial evidence that immigration enforcement affects health and health care access, increased deportations do not appear to impact hospital utilization or the treatment of more serious conditions (Hines, 2020). Recent research shows no evidence that the implementation of SC affects hospital admissions or admissions for ambulatory-sensitive conditions that could be managed in an outpatient setting, such as forms of asthma or hypertension (Kolstad and Kowalski, 2012). Focusing specifically on two states, Florida and Arizona from 2005-2014, I have analyzed data on immigration enforcement and hospital inpatient discharge records to examine the consequences of immigration enforcement for the use of health care services and admissions for preventable diagnoses among the Hispanic population.
While prior literature finds that immigration enforcement affected health insurance and health outcomes, I do not find compelling evidence that SC affected hospital utilization or access to care among the Hispanic community in Florida and Arizona. The fear of being deported may deter immigrants from seeking outpatient care, thus exacerbating preventable conditions and leading to an increase in more serious inpatient hospital visits. However, the results do not show an impact of enforcement on hospital utilization. This suggests that SC may not cause a change in behavior around managing more serious health conditions.
This may be because immigrants affected by SC were already modifying their interactions with the health care system by delaying outpatient visits, avoiding hospitals, and finding other avenues of care. It is also possible that the interactions of undocumented immigrants with public institutions are driven by perceptions of local law enforcement that are more dependent on fixed local characteristics than federal policy (Asad and Rosen, 2018).
Conclusions
Research shows that undocumented immigrants face exceptional barriers to accessing health care. External constraints like time and monetary costs and the availability of affordable health insurance affect health; however, less obvious factors may also affect health care decisions. Specifically, the fear of deportation causes stress with negative effects on health, and the concern about revealing one’s own legal status or that of a relative reduces take-up of public programs. Policy can improve these circumstances. First, de-criminalizing immigration and opening pathways to permanent residence for undocumented immigrants who have made their lives in the U.S. could reduce fear of enforcement. Second, relaxing the public charge rule, which makes immigrants who receive certain types of public benefits ineligible for legal permanent residence or citizenship, and improving health insurance coverage for the immigrants, would also increase health care access for this population.
This is particularly important in light of the recent pandemic. Although U.S. Citizenship and Immigration Services (USCIS) has noted that COVID-related testing and treatments will not be counted under the public charge rule, confusion and ambiguity have generated fear among immigrants of getting tested or treated for COVID-19 (Jordan, 2020). In addition, beyond the health of the population directly affected by immigration enforcement – undocumented immigrants and their families –health and health care access of this population has spillover effects on the rest of society. COVID-19 highlights the externalities of health care and demonstrates that barriers to health care, whether explicit or implicit, place unnecessary burdens on the system.
View and Download this Policy Brief
References
Akresh, Ilana Redstone. 2009. “Health Service Utilization Among Immigrants to the United States.” Population Research and Policy Review, 28(6): 795.
Alsan, Marcella, and Crystal Yang. 2018. “Fear and the Safety Net: Evidence from Secure Communities.” National Bureau of Economic Research Working Paper 24731.
Amuedo-Dorantes, Catalina, and Mary J. Lopez. 2017. “The Hidden Educational Costs of Intensified Immigration Enforcement.” Southern Economic Journal, 84(1): 120– 154.
Anderson, Norman B., Rodolfo A. Bulatao, and Barney Cohen (eds). Critical Perspectives: on Racial and Ethnic Differences in Health in Late Life, National Research Council 2004. The National Academies Press: Washington D.C.
Asad, Asad L., and Eva Rosen. 2018. “Hiding within racial hierarchies: how undocumented immigrants make residential decisions in an American city.” Journal of Ethnic and Migration Studies, 0(0): 1–26.
Asad, Asad L., and Matthew Clair. 2018. “Racialized legal status as a social determinant of health.” Social Science & Medicine, 199: 19–28.
Cavazos-Rehg, Patricia A., Luis H. Zayas, and Edward L. Spitznagel. 2007. “Legal status, emotional well-being and subjective health status of Latino immigrants.” Journal of the National
East, Chloe N, Philip Luck, Hani Mansour, and Andrea Velasquez. 2018. “The Labor Market Effects of Immigration Enforcement.” IZA, DP No. 11486.
Gelatt, Julia, Heather Koball, Hamutal Bernstein, Charmaine Runes, and Eleanor Pratt. 2017. “State Immigration Enforcement Policies.”
Hacker, Karen, Jocelyn Chu, Lisa Arsenault, and Robert P. Marlin. 2012. “Provider’s perspectives on the impact of Immigration and Customs Enforcement (ICE) activity on immigrant health.” Journal of Health Care for the Poor and Underserved, 23(2): 651–665.
Hines, Annie Laurie. 2020. “The Effects of U.S. Immigration Policy on Crime, Health, and Education.” Doctoral Dissertation, Economics. University of California, Davis.
Hines, Annie Laurie and Peri, Giovanni, 2019. "Immigrants' Deportations, Local Crime and Police Effectiveness," IZA Discussion Papers 12413, Institute of Labor Economics (IZA).
Jordan, Miriam. 2020. “`We’re petrified: immigrants afraid to seek medical care for coronavirus”. The New York Times. May 18, 2020: https://www.nytimes.com/2020/03/18/us/coronavirus-immigrants.html
Kolstad, Jonathan T., and Amanda E. Kowalski. 2012. “The impact of health care reform on hospital and preventive care: Evidence from Massachusetts.” Journal of Public Economics, 96(11): 909–929.
Lopez, William D., Daniel J. Kruger, Jorge Delva, Mikel Llanes, Charo Ledo ́n, Adreanne Waller, Melanie Harner, Ramiro Martinez, Laura Sanders, Margaret Harner, and Barbara Israel. 2017. “Health Implications of an Immigration Raid: Findings from a Latino Community in the Midwestern United States.” Journal of Immigrant and Minority Health, 19(3): 702–708.
Maldonado, Cynthia Z., Robert M. Rodriguez, Jesus R. Torres, Yvette S. Flores, and Luis M. Lovato. 2013. “Fear of Discovery Among Latino Immigrants Presenting to the Emergency Department.” Academic Emergency Medicine, 20(2): 155–161.
Martinez-Donate, Ana P., Xiao Zhang, M. Gudelia Rangel, Melbourne Hovell, Norma-Jean Simon, Catalina Amuedo-Dorantes, Carol Sipan, and Sylvia Guendelman. 2014. “Healthcare access among circular and undocumented Mexican migrants: results from a pilot survey on the Mexico-US border.” International Journal of Migration and Border Studies, 1(1): 57–108.
Novak, Nicole L., Arline T. Geronimus, and Aresha M. Martinez-Cardoso. 2017. “Change in birth outcomes among infants born to Latina mothers after a major immigration raid.” International Journal of Epidemiology, 46(3): 839–849.
Rhodes, Scott D., Lilli Mann, Florence M. Sim ́an, Eunyoung Song, Jorge Alonzo, Mario Downs, Emma Lawlor, Omar Martinez, Christina J. Sun, Mary Claire O’Brien, Beth A. Reboussin, and Mark A. Hall. 2015. “The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States.” American Journal of Public Health, 105(2): 329–337.
Swartz, Jonas J., Jens Hainmueller, Duncan Lawrence, and Maria I. Rodriguez. 2017. “Expanding Prenatal Care to Unauthorized Immigrant Women and the Effects on Infant Health.” Obstetrics and Gynecology, 130(5): 938–945.
Torche, Florencia, and Catherine Sirois. 2019. “Restrictive Immigration Law and Birth Outcomes of Immigrant Women.” American Journal of Epidemiology, 188(1): 24–33.
Vargas Bustamante, Arturo, Hai Fang, Jeremiah Garza, Olivia Carter-Pokras, Steven P. Wallace, John A. Rizzo, and Alexander N. Ortega. 2012. “Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status.” Journal of Immigrant and Minority Health, 14(1): 146–155.
Vargas, Edward D. 2015. “Immigration enforcement and mixed-status families: The effects of risk of deportation on Medicaid use.” Children and Youth Services Review, 57: 83–89.
Venkataramani, Atheendar S., Sachin J. Shah, Rourke O’Brien, Ichiro Kawachi, and Alexander C. Tsai. 2017. “Health consequences of the US Deferred Action for Childhood Arrivals (DACA) immigration programme: a quasi-experimental study.” The Lancet. Public Health, 2(4): e175–e181.
Wang, Julia Shu-Huah, and Neeraj Kaushal. 2018. “Health and Mental Health Effects of Local Immigration Enforcement.” National Bureau of Economic Research Working Paper 24487.
Watson, Tara. 2014. “Inside the Refrigerator: Immigration Enforcement and Chilling Effects in Medicaid Participation.” American Economic Journal: Economic Policy, 6(3): 313–338.
